HIT Perspectives
Subscribe
HIT Perspectives – January 2023
TEFCA is Gaining Momentum: Pay Attention & Get Engaged
 By Ken Kleinberg, Innovative Technologies Practice Lead
By Ken Kleinberg, Innovative Technologies Practice Lead
Quick Summary
- The final version of TEFCA. born out of the 21st Century Cures Act, was released one year ago
- TEFCA’s goal is to ensure health care providers, patients, commercial and federal payers, public services and other stakeholders have secure, single on-ramp access to EHI when and where it is needed
- TEFCA was built upon existing infrastructure largely based on the Integrating the Healthcare Enterprise (IHE®) standards initiative to which not all stakeholders adhere/utilize
- FHIR is being incorporated into TEFCA via the TEFCA FHIR Roadmap & TEFCA FHIR Implementation Guide
- To date, as many as a dozen organizations have, either applied, submitted letters of intent or stated their intention to become QHINs
- The introduction and growing use of QHINs will likely lead to changes in the current landscape of HIEs
- In addition to formal comment opportunities, the industry can get engaged with TEFCA through RCE hosted monthly information sessions
It’s been a year since the Office of the National Coordinator for Health Information Technology (ONC) released its final version of the initial Trusted Exchange Framework and Common Agreement (TEFCA). In that time, TEFCA has already proven beneficial in helping health care stakeholders move toward a more standardized and seamless approach to data access and exchange.
While the past 12 months have indeed provided ample time for interoperability growth, TEFCA has actually been in the works since being drafted in 2018. Interoperability-minded health information technology (health IT) developers eagerly tracked its progress, submitting more than 100 comments during the second draft’s public commenting period and awaiting final release in anticipation of the impact it would have on the sharing of health data.
Born out of the 21st Century Cures Act and a commensurate need to offer health care stakeholders a common set of principles, terms and conditions that enables nationwide exchange of electronic health information (EHI) across disparate health information networks (HINs), TEFCA’s end goal has always been to help ensure that health care providers, patients, commercial and federal payers, public services and other stakeholders have secure, single on-ramp access to EHI when and where it is needed. As National Coordinator Micky Tripathi pointed out in his announcement of TEFCA’s release, “The Internet has taught us that networks are more valuable together than apart. The overall goal for TEFCA is to establish a floor of universal interoperability across the country.”
Taking a closer look, TEFCA’s aim is to create a unified process that:
- Increases secure and appropriate access to EHI, helping providers to improve patient care.
- Provides individuals with easier access to their complete health history in one place.
- Supports care coordination, case management and health plan operations by reducing burdens when sharing information, such as eliminating the need to join multiple HINs.
- Improves health equity by providing information access to public health departments, alleviating the tremendous burden on providers of reporting via nondigital means or connecting with several single-purpose services to provide patient assistance.
- Protects patient data by providing HINs and health IT developers a common set of privacy and security requirements for identity proofing and authentication.
What Is the Current Status of TEFCA? 
For early adopters of the agreement, the perception of TEFCA may be that progress is slow or lagging in its use of more modern standards. That wouldn’t be too far off the mark given that TEFCA authors/collaborators were charged to fulfill the 21st Century Cures Act direction to “avoid the disruption of existing exchanges between participants of health information networks.” TEFCA, version 1, and the companion Qualified Health Information Network Technical Framework (QTF) were built upon existing infrastructure largely based on standards set by the Integrating the Healthcare Enterprise (IHE®) standards initiative to which not all stakeholders adhere/utilize. Payers, for example, typically haven’t implemented IHE. Of particular concern to health information service providers (HISPs) and their users is that use of secure direct messaging was not incorporated into TEFCA. Instead, to keep TEFCA requirements on the same foundation, IHE-based push notifications are required. Additionally, and most notably, Fast Healthcare Interoperability Resources (FHIR) was not initially required (see below).
As any health care industry participant can attest, stakeholder groups haven’t always shared the same technology paths and adoption curves, much less used the most modern standards. While TEFCA has helped the industry unify its data-sharing processes to some extent, there is still much work to be done. Providers must still join multiple HINs to access the information they need to provide proper patient care and receive reimbursement. And it is still not easy for individuals to access their own medical histories.
Such organizing bodies as the ONC and The Sequoia Project are working tirelessly to ensure that TEFCA makes an interoperability impact sooner rather than later. The Sequoia Project, a nonprofit public/private collaborative focused on interoperability efforts and well known as developer of the Carequality interoperability framework, is entering its fourth year as the recognized coordinating entity (RCE) for TEFCA, responsible for developing, implementing and maintaining the agreement that sets the baseline technical and legal requirements necessary for sharing EHI in compliance with the Cures Act.
As RCE, The Sequoia Project also designates and monitors those organizations that will eventually become certified as qualified health information networks (QHINs), per its QTF. It is also expected to collaborate with stakeholders, helping them to eventually share those same paths and curves noted above. The Sequoia Project regularly hosts information sessions to provide updates on developments and provides office hours to accommodate questions from QHIN prospects or applicants. Additional opportunities for collaboration include formal requests for information and feedback. It is expected that once TEFCA becomes more established, a more comprehensive stakeholder governance council will be created. Most recently, the RCE released updated versions of the QHIN onboarding & designation standard operating procedure and the QHIN application for stakeholder feedback (which had a due date of January 11, 2023).
Aspiring QHINs
The RCE has seen momentum grow among health care organizations expressing interest and/or applying to become a TEFCA-designated QHIN. As many as a dozen well-respected organizations have, as of publication time, either applied, submitted letters of intent or made their intention to become QHINs publicly known. They include:
- The eHealth Exchange, the nation’s largest HIN and the one most aligned with government agencies, such as the Social Security Administration. eHealth Exchange has participated in use cases and provided feedback to the RCE since its inception
- CommonWell Health Alliance, a nonprofit national network comprised primarily of health IT vendors, has also worked with the RCE to shape TEFCA
- Epic, a leading electronic health record (her) vendor, is the first in its segment to announce its intention to become a QHIN. Epic brings more than 15 years’ experience with its own Carequality interoperability framework. The Carequality team has also collaborated with the RCE to share technical experience and provide feedback on TEFCA standards. Other EHR vendors with QHIN aspirations include NextGen and Netsmart
- Health care technology vendors Health Gorilla and Kno2 have both begun the QHIN application process
- MedAllies is one of the few HISPs intending to become a QHIN
- KONZA National Network, is the first health information exchange (HIE)-oriented organization (operating in multiple states) to move toward QHIN designation
- eHealth Exchange and Consortium for State and Regional Interoperability (CSRI) recently announced a QHIN partnership
Once the RCE and ONC have approved an application, the actual testing process for a QHIN can take up to a year. Facilitated, open data exchange among QHIN participants and their network subparticipants is planned for mid-to late 2023 but may not become a reality until 2024. It is possible that some organizations will not succeed in their first attempt toward QHIN designation. QHIN designees may also lose their privileges for nonperformance.
From Applicant to Impact Maker
Health Gorilla Chief Medical Officer Steven Lane, MD, shared during a recent Point-of-Care Partners Dish on Health IT Podcast that he believes the interoperability platform company’s future QHIN status will help it become even more of a vehicle for innovation. Dr. Lane, who is also a practicing family physician having extensive experience with federal interoperability efforts, likened a QHIN to building a dance studio — a safe space where individuals, couples or dance troupes can come and perform whatever dance (data exchange) they like, whether it be the cha-cha, merengue, ballet or breakdancing. We’ll let you decide which dance corresponds with what type of data exchange. Each QHIN applicant will have its own strategic reasons for applying. Lane pointed out that organizations voluntarily signing up for even more government oversight must clearly see it as a viable way to take a substantial step forward in their interoperability efforts.
What’s Next?
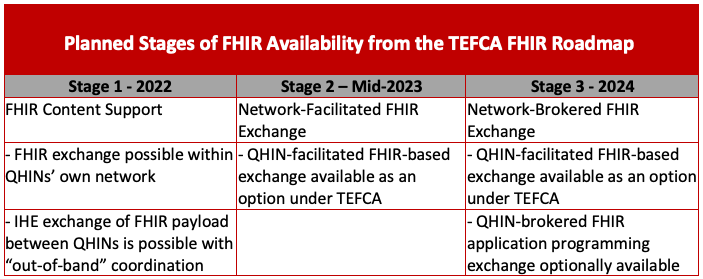
As previously mentioned, TEFCA has taken a conservative approach to new standards and technology when it comes to QHIN-to-QHIN exchange, initially relying on the existing IHE-based networks while drafting standards and implementing use cases (also known as exchange purposes). The growing adoption of FHIR has increased focus on ways to integrate or develop parallel paths that allow QHINs, participants and subparticipants to exchange information using FHIR standards.
The FHIR Roadmap for TEFCA Exchange, version 1, released in January 2022, the TEFCA Facilitated FHIR Implementation Guide, Draft 1, released in October 2022, and Draft 2, released in December 2022, demonstrate RCE recognition of the need for further collaborations to take into account future use cases and/or TEFCA FHIR pilots.
At least 16 industry-leading entities provided responses to the request for feedback about FHIR+, including CommonWell, eHealth Exchange, Epic and HL7’s FAST accelerator. Several common themes emerged in their feedback, with a shared concern being the lack of alignment between the previously released TEFCA FHIR Roadmap and how the TEFCA Facilitated FHIR Implementation Guide provided more of a capabilities overview than actionable steps for implementation.
Other frequently mentioned concerns involve public health query capabilities and patient matching being limited to $match. Feedback also reflected the need for more clearly defined roles among actors and an established process to verify, validate and certify end points among them. Reviewers also mentioned the need for more detail in describing clinical data exchange, provenance, consent, Health Information Portability and Accountability Act compliance and QHIN certification management.
Taken as a whole, the responses reveal growing demand to incorporate FHIR into the TEFCA framework but that the process for doing so will take years to implement. Responses to the TEFCA Facilitated FHIR Implementation Guide are available here.
Future Exchange Purposes and Ways to Become Involved
Initially, TEFCA will focus on data exchange for treatment purposes and individual access services. Additional exchange purposes are expected to include public health, government benefits determination and payment and health care operations. The degree to which TEFCA may someday overlap with the realm of clearinghouses is a subject of interest to many in the payer community, who may not feel that TEFCA is doing enough for their interests.
For the time being, TEFCA participation will remain voluntary. To date, the only incentives for becoming a QHIN are driven by market advantages and the potential for offering improved information exchange. While there are no fees for applying to become a QHIN, there is a substantial investment in resources (and there will likely be some ongoing RCE fees at some point), so many organizations are taking a wait-and-see approach. The introduction and growing use of QHINs will likely lead to changes in the current landscape of HIEs. Redundancies and potential disintermediation may lead to mergers between HIEs, while some will determine that it is more beneficial to become a QHIN.
There are also no federal advantages to becoming a TEFCA participant or subparticipant, although participation could help an organization demonstrate it is not engaging in information blocking. It is possible that future regulations could make TEFCA a requirement for some Medicare or Medicaid programs, with commercial payers potentially following suit.
The RCE will continue hosting monthly information sessions throughout 2023. Information about attending and opportunities to submit requests for feedback can be found on the Sequoia website here.
Point-of-Care Partners regularly assesses the resources developed for TEFCA and provides strategic insights for improved collaboration. If you have questions about TEFCA and how the rollout of a national QHIN network may affect your organization in 2023, please reach out to me at ken.kleinberg@pocp.com.
UPDATE: Since publishing this article, HHS announced it will recognize organizations approved for onboarding as Qualified Health Information Networks (QHINs) under TEFCA on Monday, February 13, 2023, from 11AM-12:30PM ET. To join the event, use this link: https://hhs.gov/live




