HIT Perspectives
Subscribe
HIT Perspectives – November 2023
Advancing Pharmacy Practice: Bridging Policy, Value-Based Care Models, Technology and Health Equity
 By Pooja Babbrah, Pharmacy & PBM Practice Lead
By Pooja Babbrah, Pharmacy & PBM Practice Lead
Quick Summary
-
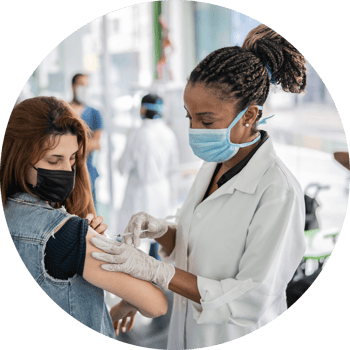
Evolution of Pharmacy Services: Trace the transformation of pharmacist roles from traditional tasks to providing expanded services like administering vaccines, conducting point-of-care testing, and even considering a move into primary care, all while embracing digital data sharing.
-
Rise of Community Pharmacies: Explore the growing reliance of patients, especially in underserved rural areas, on community pharmacies for accessible healthcare services, underscoring the shift in patient behavior towards pharmacist involvement in their care.
-
Role of Pharmacists in Filling Healthcare Gaps: Understand how pharmacist involvement becomes crucial as primary care provider shortages persist, particularly in rural areas, showcasing their vital role in providing ongoing care for patients with complex medical needs.
-
Policy-Driven Expansion: Delve into the dynamic policy environment that's reshaping the scope of pharmacy practice, especially in vaccine administration, diagnostic testing, and prescribing authority, driven by both state and federal policies.
-
Technological Enablement: Discover the pivotal role of technology in empowering pharmacists, ensuring data interoperability, enhancing clinical excellence, and supporting health equity initiatives within the evolving healthcare landscape.
-
Embracing Collaborative Care: Highlight the growing consensus among healthcare professionals about the effectiveness of team-based care, showcasing how collaborative practice agreements and value-based care models are reshaping the role of pharmacists.
-
Navigating Reimbursement Challenges: Address the critical issue of reimbursement for pharmacists' expanded roles, exploring how business models are evolving, and pharmacists are strategizing to ensure sustainable growth and service delivery.
-
Pharmacy's Transformative Future: Envision the exciting possibilities for pharmacy practice, driven by policy shifts, technology adoption, and evolving care models, positioning pharmacists as essential care providers in a patient-centered healthcare system.
In the ever-evolving landscape of healthcare, the role of pharmacists has seen a remarkable transformation. From the oldest known prescriptions recorded on clay tablets in Mesopotamia to the establishment of pharmacy guilds in the 17th century and the launch of the American Pharmaceutical Association 200 years later, pharmacists have long been recognized as respected providers of care within their communities.
Correspondingly, there has over time been a significant shift in how patients access that care, due in large part to healthcare policy changes and technological advances. The clamor of patients for easier access to higher-quality, more affordable care has led pharmacists to expand their services beyond the traditional ones of yesteryear. While the Mr. Gower of Bedford Falls may have spent most of his time filling capsules and delivering medicines to the homes of patients like the Baileys, his modern-day counterpart is now busy administering vaccines, offering point-of-care testing, monitoring medications and reviewing therapy regimens. Today’s pharmacists are even considering expanding into primary care. And most, if not all, are now digitally sharing patient encounter data upstream and down.
Patients, particularly those in underserved rural areas, are more frequently turning to their local pharmacies (rather than the local health system) for more easily accessible healthcare services – a trend that makes sense given that 90% of the United States (US) population lives within five miles of a community pharmacy. It should also come as no surprise that patients visit these pharmacies 12 times more often than they do their family physicians, according to research from Wolters Kluwer Health, which also finds that 61% of people believe that pharmacies, retail clinics or pharmacy clinics will begin providing primary care within the next five years. Add the fact that over half of the surveyed population say they’d trust a pharmacist to prescribe medications if it resulted in cost savings, and it becomes crystal clear that patients have embraced the idea of pharmacists as integral members of their care teams.
As physician shortages continue, economic constraints linger and typical healthcare service access points dry up, healthcare organizations will quickly realize that expanding and/or integrating pharmacy services into their clinical and business workflows will be essential to patient and member satisfaction, not to mention the bottom line.
Looking at it one more level down, this means that payers will need to evaluate their coverage strategies and assess the technology and data exchange needs to support it. Health tech vendors will need to be proactive and consider how their solutions can bridge different clinical settings, including pharmacy, as pharmacy clinical offerings grow. Providers, who have already been establishing service agreements with local pharmacists, will need to continue evolving and leveraging those pharmacy relationships to best serve their communities while simultaneously prioritizing the services they offer so that providers – whether physician, nurse practitioners or physician assistants – can operate at the top of their licenses.
What’s Driving the Need to Expand Pharmacist Capabilities?
It’s no secret that staffing shortages are exacerbating healthcare access issues across the country. Pharmacists are stepping in to fill crucial gaps in patient care as primary care provider shortages worsen. According to recent data from Surescripts, there is just one primary care physician for every 1,500 people in nearly half of counties within the US. Thus, almost by default, pharmacists are already having to care for patients with chronic conditions, offering a lifeline to those in need of regular care management and underscoring the critical role they are poised to play in ensuring continued care for patients with complex medical needs.
Patients in rural and underserved areas have also come to increasingly rely on their community pharmacies for care that in more metropolitan areas would typically be provided by physicians. Patients in these areas, served by these types of pharmacies, gain improved access to care without the need for lengthy and costly trips to distant medical facilities.
As rural areas face a continuing shortage of family care physicians and healthcare deserts continue to expand, community pharmacies are poised to play important, collaborative roles in health equity programs, ensuring increased access to care in areas that have typically gone without.
Policymakers Are Enabling the Shift
It’s crucial to acknowledge the dynamic policy environment driving the shift toward expanded pharmacy services. Policies at both the state and federal levels have been pivotal in redefining the scope of practice for pharmacists. This expansion is highlighted by several key trends in vaccine administration and diagnostic testing. According to the National Alliance of State Pharmacy Associations (NASPA), pharmacists can now administer flu vaccines in all 50 states and coronavirus vaccines in 49 states. Pharmacists are also increasingly engaged in diagnostic testing, with bipartisan federal efforts already in the works to ensure Medicare patients have access to these types of pharmacy-based services. A notable policy brief by the Mercatus Center delves into the positive implications of broadening pharmacists' prescriptive authority and serving populations who may not have easy access to primary care in any form.
When it comes to prescribing medications, however, the specifics of pharmacist authority vary substantially based on medication type and state regulations. For example, legislators in 24 states and Washington, DC have empowered pharmacists to prescribe contraceptives. In 2022, 178 bills related to pharmacist scope of practice and payment were introduced in 38 states, according to NASPA. Sixteen states took definitive steps to expand services provided by pharmacists. Our Regulatory Resource Team has tracked 113 active bills related to pharmacist scope of practice in 2023, so policy activity appears to be at a consistently high level.
While these state-level policy changes are vital, they often occur incrementally, state by state. To fully unlock the collaborative benefits that pharmacists can bring to patient care, a comprehensive national policy shift is imperative. Significant policy changes may take time at this level, however, due to the complex nature of healthcare policy and diverse array of interests involved.
Though federal policymaking may lag, momentum at the state level is setting the stage for a more cohesive, collaborative and efficient healthcare system. This wave of legislative action demonstrates a collective recognition of the potential for pharmacists to be essential members of patient care teams.
Technology Is Following Suit
The expanding role of pharmacists will gain even more momentum as they and their fellow healthcare collaborators recognize and invest in necessary technological underpinnings. Harnessing technology and fostering interoperability across all healthcare environments, inclusive of pharmacy settings, are becoming more essential to achieving clinical excellence and advancing health equity. This shift and growing need will have a ripple effect impacting stakeholders across the ecosystem, not just pharmacists and pharmacies.
As pharmacists increasingly take on more primary care-related tasks, their need to document medication-related problems and other patient care activities will only grow, as will the need to share their data throughout their pharmacy’s healthcare system – whether that be with the health system up the street, physician’s office around the corner or a patient’s telemedicine provider. The implementation of interoperable systems is poised to simplify the exchange of data amongst a patient’s care team, ensuring that patients, physicians, social care service providers and even family caregivers have access to and can share data in nearly real time.
Payers, too, are increasingly acknowledging the invaluable contributions pharmacists are poised to make in areas such as screenings, medication management, health equity initiatives and facilitating access to member benefits. They are also realizing the impact digital data exchange with pharmacists will have on the aforementioned areas. Having the right data at the right time will better enable pharmacy teams to fill access gaps with necessary clinical services and enhance and measure the progress of a payer’s health equity efforts, ultimately affording pharmacist and payer more time for personalized and timely interactions with patients and plan members.
Up-to-date digital documentation systems and accompanying analytics, data-sharing capabilities and even the relatively new area of telepharmacy will be critical to helping pharmacists understand patient outcomes and, in turn, helping them showcase their value within the healthcare system.
Federal and trade association efforts are already underway to help ensure pharmacists are brought into the data-sharing fold. In early 2023, the Office of the National Coordinator for Health Information Technology (ONC) established the Health Information Technology Advisory Committee Task Force on Pharmacy Interoperability and Emerging Therapeutics to gather recommendations for supporting seamless information exchange between pharmacies and other care settings in support of medication management, patient safety and consumer engagement. I was honored to be a member of this task force and commend ONC for making pharmacy interoperability a priority and focus. You can read the recommendations report that was presented on the November 9th public call here: https://www.healthit.gov/sites/default/files/facas/2023-11-09_PhIET_TF_2023_Recommendations_Report_0.pdf
The National Council for Prescription Drug Programs is also supportive of the critical role innovations within the pharmacy sector will play in advancing clinical excellence and promoting health equity. It has several projects in the works to ensure this progress continues, including its Care Coordination and Innovation Workgroup. Launched just several months ago, the group aims to play a pivotal role in fostering excellence and innovation in pharmacy practices.
Technology adoption will be instrumental in helping pharmacists achieve clinical excellence and advancements in health equity. As the healthcare landscape continues to evolve, embracing innovative digital solutions within the pharmacy setting will become essential to delivering the best possible care to patients from all walks of life.
 Healthcare Stakeholders Are Slowly but Surely Embracing the Shift
Healthcare Stakeholders Are Slowly but Surely Embracing the Shift
There is a growing body of evidence that indicates healthcare professionals, including 89% of prescribers and 97% of pharmacists, understand the pivotal role team-based care plays within the healthcare system. This consensus highlights a shared belief in the potential of collaboration to enhance patient care and outcomes.
Collaborative practice agreements, which have been adopted in all 50 states and Washington, DC, offer patients low-cost medical testing and treatment options. Through these agreements, patients can bypass costly visits to physicians and receive more timely care from pharmacists for conditions with straightforward diagnoses and treatments. Studies have indicated that this streamlined approach, which also offers reimbursement advantages, can yield substantial savings, particularly when it comes to routine and easily treatable illnesses.
The integration of pharmacy and primary care has piqued the interest of not only retailers like Walmart, CVS and Walgreens but also community pharmacists, many of whom are moving toward value-based care models. Programs like Flip the Pharmacy have been instrumental in this transition. Launched by the Community Pharmacy Foundation and the Community Pharmacy Enhanced Services Network, FtP is leading the way in transforming community pharmacies into easily accessible, value-based care destinations that focus on social determinants of health, opioid stewardship, immunizations and enhanced clinical services.
Making This New, Collaborative Business Model Work
The question of reimbursement must be addressed if pharmacists are truly going to become invaluable members of patient care teams. Pharmacists have experienced significant operational changes in recent years, driven by a combination of buyouts, consolidation and diversification into new business lines. These shifts have transformed the landscape of pharmacy ownership and have implications for business sustainability, not to mention service delivery and accessibility.
While value-based agreements are slowly but surely gaining in popularity and practice, many pharmacists face challenges in establishing and executing these types of arrangements, especially with health plans. Pharmacists instead are entering into collaborative practice and compensation agreements with local physicians to ensure reimbursement.
Business-savvy pharmacists are redefining their roles amidst shifting business models, navigating the complexities of the healthcare reimbursement system and exploring new avenues for sustainable growth and service delivery. The changes in pharmacy ownership and adoption of these collaborative agreements are integral components of this evolving scope-of-practice landscape.
Payers can strategically enhance their reimbursement and value-based agreement strategies by integrating pharmacists into the care team. This multilayered approach addresses health equity concerns by extending pharmacy clinical care services to underserved areas. Simultaneously, in fields like oncology, cardiology and others with high trial-and-error components, pharmacists with pharmacogenomics expertise play a pivotal role. This integration not only improves patient care and outcomes but also prevents unnecessary costs, contributing to a more effective and equitable healthcare system.
Pharmacy’s Future Is Bright
The future of pharmacy practice holds exciting possibilities – especially for patients – driven by dynamic shifts in healthcare policy, value-based agreements, technology and health equity initiatives. With pharmacies emerging as crucial pillars of the healthcare system, the industry is poised for transformative growth. The expansion of pharmacists’ roles from immunizations and chronic care management to becoming hubs for primary care positions them as essential care providers.
Pharmacy practice is becoming more patient-centered, accessible and integrated into the broader healthcare environment. As the industry continues to evolve, the role of pharmacies and pharmacists is set to become even more prominent, contributing to comprehensive, value-driven care.
For organizations seeking guidance on how these transformative policies and practices may impact their operations, Point-of-Care Partners, with its deep expertise and advocacy in health information technology consultancy, is poised to provide valuable insights. To better understand how your organization can strategically leverage these changes, consider reaching out to me at pooja.babbrah@pocp.com or the Regulatory Resource Center Lead, Kim Boyd at kim.boyd@pocp.com. The future of pharmacy practice is bright, promising a more inclusive, accessible and patient-centered healthcare system.




